Why do I need a liver resection?
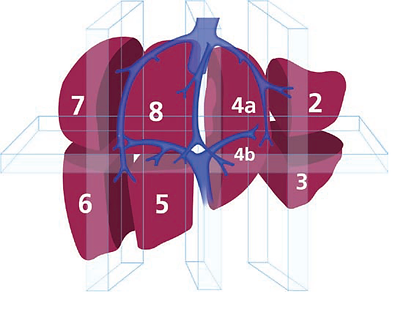
Liver resection is offered to patients who have or are thought to have a tumour (growth) on the liver. A tumour is an abnormal growth of cells and may be described as malignant (cancerous) or benign (non–cancerous). You may also be offered a liver resection if you have already had a bowel operation for bowel cancer and been found to have liver metastases (secondary cancer cells in the liver). The diagram below will be used to show you where
your tumour/s is. The liver is divided into eight segments and the detailed knowledge of the liver allows your Surgeons to plan your operation.
The surgeon will discuss with you the exact operation in more detail. You will have already undergone many tests and investigations. The results of these tests have been looked at carefully by a team of specialists known as the Multi-Disciplinary Team (MDT). This team includes Consultant Surgeons, Consultant Physicians, Consultant Radiologists (experts in taking and reading X-rays and scans) and Clinical Nurse specialists. The team has been able to make a diagnosis of your condition/illness, and a decision made about how best to treat it. As a result, they have suggested that
you have a liver resection. This will have been discussed with you. Only a relatively small number of patients with liver tumours are suitable for surgery, and whether or not this operation is an option for you depends on:
• Whether the tumour in your bowel has been treated/
is treatable.
• How much of the liver is affected.
• The size of the tumour(s).
• Where in the liver the tumours are located.
• Whether there are any tumours outside the liver.
• Your general level of fitness.